Abnormal gut microbiota can contribute to anxiety disorders and depression

The human body is home to nearly 100 quintillion bacteria that are essential to health. Their role in digestion is widely known, but recent studies have shown that the intestinal flora also plays an important role in brain function and may play a role in the development of anxiety and mood disorders.
The gut-brain axis is a two-way connection between the intestinal flora and the central nervous system. The gut microbiota can cause changes in the functioning of the digestive system, central nervous system, autonomic nervous system and immune system. Changes in the functioning of these systems, in turn, can affect fat storage and energy balance, gastrointestinal barrier function, low-grade chronic inflammation, increased stress responsiveness, and increased anxiety and depressive behavior. These are complex relationships that scientists are just beginning to understand.
Most of the knowledge about the functioning of the gut-brain axis and its influence on behavior comes from studies in mice and rats.
The gut flora influences the functioning of the hypothalamic-pituitary-adrenal (HPA) axis. In sterile mice, i.e. mice that developed under sterile conditions from birth and therefore did not develop a bacterial flora, confinement in a small space causes a greater increase in corticosterone and adrenocorticotropin (adrenal hormones involved in the stress reaction) than in ordinary mice. Thus, the bacterial flora has an impact on functioning in stressful conditions, but also stressful conditions have an impact on the bacterial flora. Separating young rats from their mothers causes long-lasting changes in the composition of their intestinal microflora, which may be one of the reasons for their greater reactivity to stress. It has also been shown that treatment with probiotic bacteria in such rats normalizes corticosterone levels and reduces depressive behavior.
Stress increases the permeability of the intestine, allowing bacteria to travel through the intestinal mucosa to the cells of the immune system and the cells of the intestinal nervous system. In this way, the bacteria can then affect the central nervous system. Moreover, it has been shown that prophylactic administration of Lactobacillus bacteria to rats prior to exposure to stress reduces the permeability of the gut which normally occurs in response to a stressful situation.
In addition to modulating the function of the HPA axis, the intestinal microflora can also directly influence the central nervous system by activating the vagus nerve. During infection with food pathogens, expression of the cFOS proto-oncogene, which indicates the activity of neurons, has been observed in sensory neurons of the vagus nerve. The same gene was expressed in certain regions of the brain.
Interestingly, several studies have shown that sterile mice, despite having elevated levels of stress hormones, exhibit less anxiety in behavior (e.g. they are more likely to be outdoors) than mice with normal bacterial flora. Later studies showed that the level of anxiety in behavior depends on the specific bacterial flora of a given mouse strain. When sterile Swiss Webster mice were colonized with Balb / C bacteria, an increase in anxiety in their behavior was observed, reflecting the typical behavior of Balb / C mice. However, when sterile Balb / C mice received their flora from Swiss Webster mice, which are generally less fearful, their anxiety was reduced.
In the studies, anxiety in Balb / C mice was also reduced by administering probiotic bacteria of the Lactobacillus genus. On the other hand, infection with pathogenic bacteria increases the anxiety behavior of mice.
So far, no experimental studies have been conducted involving people with anxiety or depressive disorders, therefore it cannot be determined whether probiotic bacteria are an effective treatment for such disorders. However, studies have been carried out on healthy volunteers and it has been shown that in such people, probiotics reduce stress and improve mood, and also affect the activity of the areas of the brain responsible for emotions.
Moreover, correlation studies have shown that the bacterial flora of people with depression contains more bacteria of the order Bacteroidales and fewer bacteria from the family Lachnospiraceae than the microflora of healthy people.
It is possible that people with depression have an increased gut permeability which causes bacteria to move around and, as a result, become inflamed in the body. This is indicated by the increased level of IgM and IgA antibodies to lipopolysaccharides present in the cell membrane of intestinal bacteria.
References:
- Foster J.A., McVey Neufeld K.A. (2013). Gut–brain axis: how the microbiome influences anxiety and depression. Trends in Neurosciences, 36(5), 305-312. (pdf na ufl.edu)
- Luna R.A., Foster J.A. (2015). Gut brain axis: diet microbiota interactions and implications for modulation of anxiety and depression. Current Opinion in Biotechnology 32, 35-41.
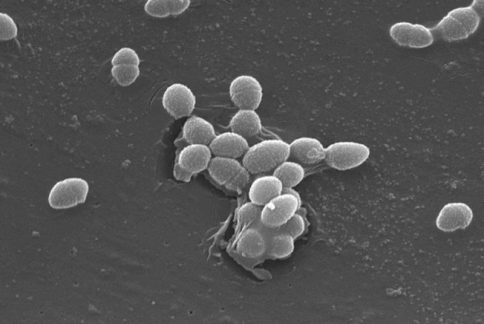
Source of picture: Autor: Janice Haney Carr. Przekazał: CDC / Pete Wardell [Public domain], za pośrednictwem Wikimedia Commons
Author: Maja Kochanowska






Add comment